In a recently published paper [1], Dr. Maria Jasmin Jamora of the Skin and Cancer Foundation, Inc. reported the use of immunofluorescence techniques in the diagnosis of blistering diseases of the skin and other dermatologic conditions. Immunofluorescence techniques and other immunopathologic diagnostic techniques in dermatology involve the detection and localization of specific autoantibodies against various antigens within the skin. Since the 1960s when the lupus band test was utilized to diagnose lupus erythematosus, diagnostic immunopathologic techniques, when interpreted alongside clinical and histopathologic findings, have become a part of the diagnostic criteria in the diagnosis of many skin diseases, in particular the autoimmune blistering diseases and connective tissue diseases.
| MARIA JASMIN J. JAMORA, MD, FPDS
Dr Maria Jasmin J. Jamora graduated from the University of the Philippines College of Medicine with a Degree in Medicine, recognized as an Outstanding Medical Graduate. She received clinical honors as outstanding intern in 4 departments. She completed a postgraduate year in Internal Medicine at the Montefiore Medical Center of the Albert Einstein College of Medicine of Yeshiva University in the Bronx, New York. She finished her dermatology residency at the Skin and Cancer Foundation, Inc. in Manila Philippines and became the Chief Resident. She passed her Diplomate Boards of the Philippine Board of Dermatology and is currently a Fellow in good standing of the Philippine Dermatological Society, the official affiliate subspecialty society of the Philippine Medical Association. Dr. Jamora completed a year of research fellowship at New York University Medical Center in Immunodermatology and Immunofluorescence Techniques under the tutelage of Prof. Jean-Claude Bystryn, where they published articles in the Archives of Dermatology, Journal of the American Academy of Dermatology and the International Journal of Dermatology. She then completed a fellowship year at the Indiana University School of Medicine in Dermatopathology with Profs. Antoinette F. Hood and Dr. William B. Moores, and published an article in the Archives of Facial Plastic Surgery. She became assistant training officer and is currently Residency Training Officer of the Skin and Cancer Foundation, Inc. dermatology training program. She is also active staff and Faculty teaching clinical dermatology and Dermatopathology for the Dermatology Departments of Makati Medical Center and St Lukes Medical Center. She is visiting faculty at Quirino Memorial Medical Center. She is also a practicing clinical dermatologist, dermatopathologist and immunopathologist at all three institutions. |
The article, which appeared in the December 2008 issue of Dermatologica Sinica, gives an overview of basic and updated immunopathologic techniques used in the diagnosis of many dermatologic conditions, based on the pattern of immunofluorescence staining. For instance, epidermal intercellular staining encompasses the pemphigus group and its variants, while keratinocyte cell surface staining with dermoepidermal junction staining leads to the diagnosis of paraneoplastic pemphigus. Staining of the basement membrane zone points to the diagnosis of the subepidermal blistering diseases, including the pemphigoid group and variants, epidermolysis bullosa acquisita, linear IgA bullous dermatosis or dermatitis herpetiformis. Shaggy fibrinogen staining at the basement membrane zone with cytoid bodies is characteristic of lichen planus. Vascular staining may help diagnose immune complex vasculitis, and homogeneous vascular staining combined with dermoepidermal staining suggests the diagnosis of porphyria cutanea tarda.
Some of the assays identified in the paper includes the ELISA using the NC16a domain of bullous pemphigoid antigen-2 (180 kDa), which is an important adjunct tool in the diagnosis of bullous pemphigoid, mucous membrane pemphigoid, anti-epiligrin cicatricial pemphigoid, lichen planus pemphigoides and pemphigoid gestationis. The ELISA utilizing the NC1 domain of type VII collagen was found to be relevant in the diagnosis of bullous systemic lupus erythematosus and epidermolysis bullosa acquisita. In dermatitis herpetiformis, the use of both the indirect immunofluorescence method to detect IgA anti-endomysial antibodies and the tissue transglutaminase, ELISA increases diagnostic sensitivity. In the diagnosis of necrotizing vasculitis, ELISAs using cardiolipin have been developed to detect antibodies in Henoch-Schonlein purpura, while ELISAs using proteinase-3 and myeloperoxidase were studied for the diagnosis of Wegener’s granulomatosis. The differential diagnosis of other immunofluorescence patterns like cytoid bodies, epidermal nuclear fluorescence are also discussed.
The paper also discussed the significance of other patterns of staining like cytoid bodies (found in interface dermatitis like lichen planus and lupus erythematosus), and anti-nuclear fluorescence (seen in mixed connective tissue disease). A detailed explanation of clinical features, common immunofluorescence findings and adjunctive immunopathologic techniques like immunoblotting is also given.
The advancement of current knowledge at the molecular level is rapid, leading to the precise identification of target antigens, and production of recombinant proteins used in enzyme-linked immunosorbent assays (ELISA). These assays are highly sensitive and specific tests that calls into question the relevance of more traditional immunofluorescence techniques. Although the use of direct and indirect immunofluorescence, salt split skin technique, immunoelectron microscopy and immunoblotting remains relevant and often served as first-line diagnostic tools, recently developed enzyme linked immunosorbent assays (ELISA) utilizing recombinant proteins to detect serum antibodies demonstrate high sensitivity and specificity in many skin conditions.
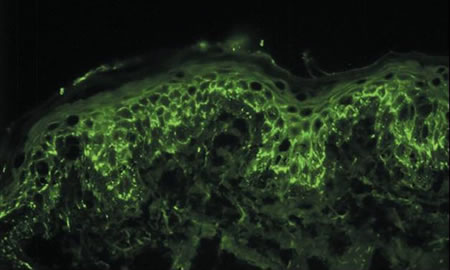 Intercellular staining of epidermal skin cells with fluorescent markers in a patient with pemphigus vulgaris using direct immunofluorescence. |
Reference:
[1] Jamora, MJJ, Diagnostic Immunopathology in 21st Century Dermatology Part II: Basement Membrane and Vascular Reactions, Dermatol Sinica 26: 191-227, 2008.